Proposed Program to Reduce the Incidence of Cervical Cancer in Pakistan
Program aim:-
“To reduce the incidence of cervical cancer in Pakistan.”
Program Objectives:-
By the year 2020,
-To vaccinate girls 09-14yrs against HPV 16 & 18.
-To include HPV vaccination in the routine vaccination programs for children.
-To register marriages only if the bride is vaccinated against HPV 16 & 18.
-To screen married women for cervical cancer via Pap smear at an interval of 05years.
-To make sure that each woman has been screened for cervical
cancer at least once by the age of 35yrs.
Target Group:-
Women of reproductive age i.e. 18-45yrs
PRECEDE-PROCEED MODEL
FOR HEALTH PROMOTION REGARDING CERVICAL CANCER (Green & Kreuter, 1999)
1. Assessment of need and assets of the population:-
According to WHO half a million women will die of cervical cancer all over the world by 2030 and 98% of such deaths will occur in developing countries like Pakistan. Pakistan is 8th amongst the South Asian countries for the incidence of cervical cancer (ICO HPV Information Centre, 2016). Cervical cancer ranks 3rd of the cancers of women in Pakistan and is the second common cause of cancer in women age 15 to 44 years (ICO HPV Information Centre, 2016).Pakistan has neither screening nor vaccination program against HPV.
HPV types 16 and 18 are responsible for causing 70% of the cervical cancers worldwide (ICO HPV Information Centre, 2016). Vaccines for the prevention of HPV 16 and 18 are now available and are effective against the prevention of cervical and anogenital cancers caused by HPV (ICO HPV Information Centre, 2016).
The tangible assets that we have here in Pakistan are the vaccination centers, the District Headquarters Hospital (Obs. & Gynae. Units), the Rural Health Centers, the Reproductive Health Service Centers and the Family Welfare Centers (at the level of the union council). The intangible assets that we have are the Lady Health Workers, Family Welfare Workers and the Lady Doctors.
2.
Assessment of causes, setting priorities,
aims and objectives:-
Phase I Social
Assessment (Green & Kreuter, 1999)
In this phase women of reproductive age will be asked how they
perceive their gynecological problems and what their priorities are when it
comes to examination, vaccination, treatment etc.
Phase
II Epidemiological Assessment (Green
& Kreuter, 1999)
According to 2012 estimates 5233 new cases of cervical cancer are diagnosed annually in Pakistan and about 2876 women die of cervical cancer annually (ICO HPV Information Centre, 2016). It is the 5th leading cause of cancer deaths in women in Pakistan (ICO HPV Information Centre, 2016).
Phase
III Educational and ecological
assessment (Green & Kreuter, 1999)
Predisposing
factors
-Early marriages in Pakistan are one of the leading causes of
cervical cancer. According to Pakistan Demographic Health Survey 2012-13, the
median age of marriage for women in Pakistan is 19.5 years and the median age
of having first baby is 22.2 years.
-4% women and 3% men are in a polygamous relationship in Pakistan,
as polygamy is legal here for men (PDHS, 2012-13).
-Extra marital sex (Heterosexual and homosexual) and prostitution
is also common, although relevant data is not available because it is not
openly talked about (Pal Ahsan Sadia,
2015). Cigarette smoking, Shisha, chewing tobacco ‘Naswar’ and betel leaves
‘pan’ is also common though relevant data is not available (Pal Ahsan Sadia,
2015).
-In Pakistan cervical cancer is mostly
caused by HPV 16 and 18. In a small pilot study at Karachi, Pakistan out of the
91 women having invasive cervical cancer, 88% were HPV 16 and 18 positive,
75.8% had
HPV 16, 6.6% had HPV 18 and 4.4% were positive for HPV 45 (Raza et al, 2010).
-The
literacy rate of women in Pakistan is very low i.e. 57% (Economic survey of
Pakistan 2009-10); hence they are unable to understand their health problems
effectively. The female literacy rate is 45% and for males is 69% (Economic
survey of Pakistan 2009-10)
-The
dominance of males and the in laws (especially mother in law) also hinders
women from seeking medical help, as most of the time they are not supportive.
Priority will be given to screening
followed by vaccination against cervical cancer.
3.
Designing and Implementing the program:-
Phase
IV a Intervention Alignment (Green
& Kreuter, 1999)
Enabling
factors:-
-The educational intervention will be
to educate young girls and women in schools and colleges regarding cervical
cancer and its prevention via vaccination and screening.
- Discourage early marriages
-Practice safe sex
-Lady Health Workers will be trained
to disseminate the message to women for the importance of cervical screening
every 5 years and vaccinating their daughters for HPV and practice safe sex and
family planning.
-Involvement of male partners and in
laws
-Second step is towards preventing
cervical cancer via vaccination and screening. The suggested protocol for Cervical Cancer Prevention is as follows:-
“Primary Prevention:
HPV Vaccination”(Romanovski et al,
2014)
Dosage for Bivalent Vaccine:
2 dose regimen: 0 & 6 months for
girls 9-14 yrs (in school or just before leaving school)
3 dose regimen: 0, 1 & 6 months,
for girls 15 -26 yrs of age, preferably before marriage.
Dosage for Quadrivalent Vaccine:
3 dose regimen: 0, 2 & 6 months,
for girls 9-14 yrs (in school or just before leaving school).
Either of the two available vaccines
may be employed.
“Secondary Prevention”
Married women should undergo regular
Pap smear or VIA screening at an interval of 5 years (Pal Ahsan Sadiah, 2014).
Every woman should have at least one Pap smear or VIA screening by the age of
35 years (Pal Ahsan Sadiah, 2014). After 65 years of age screening is not
required, if previous screenings were normal and there are no risk factors (Pal
Ahsan Sadiah, 2014)
-Vaccination against HPV must be added
to the child’s routine vaccination programs (WHO, 2009)
-Vaccinating males is not recommended,
as vaccinating more than 70% of girls are more cost effective than vaccinating
both girls and boys (WHO, 2009)
-Special fund must be allocated to
this program for buying vaccines and kits for Pap smear according to the
women’s population covered in each union council
- Every woman above 35 years of age
visiting the hospital must be advised a Pap smear in the Reproductive Health
Service facility.
Phase
IVb Administrative and policy assessment (Green
& Kreuter, 1999)
There is no organized screening or
vaccination program for cervical cancer in Pakistan. Only ‘opportunistic
screening’ is taking place, missing under privileged women who are at a higher
risk of cervical cancer (Pal Ahsan Sadiah, 2014). The Asian Cervical Cancer
Prevention Advisory Board (ACCPAB, 2009) is of the opinion that preventive
services must be adopted with a view point to protect all women and that every
Asian woman must be vaccinated against HPV before initiating sexual activity
i.e. getting married.
Reinforcing
factors:-
-Giving allowance to the LHWs who
bring in largest number of women from their union council for vaccination and
screening
-Awarding the service delivery outlet
with the ‘best outlet’ award which provides the services of vaccination and
screening
-Giving travelling and daily
allowances to those who opt for training for the screening program
4.
Evaluation of the program:-
This health promotion program will be evaluated by using the following six steps (Prevention and Population Health Branch, 2010):-
i-
Describing the program(Prevention &
Population Health Branch, 2010)
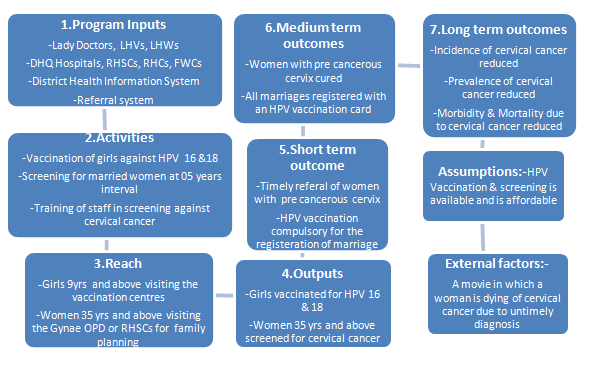
I will describe the program by using the following program logic model (Craig et al., 2008)
ii- Evaluation preview (Prevention & Population Health branch, 2010)
-Involving stakeholders
a. Lady Health Workers
b. Girls 09-14yrs and women 18-45yrs
c. Lady Doctors
d. Policy makers/authorities
The purpose of evaluation is to evaluate the outcome and the process of health promotion
-Key evaluation questions (RE-AIM) (Prevention & Population Health Branch, 2010)
a. Was the Reach of the program enough?
b. Was the program Effective?
c. Was the program Adopted by the community?
d. Was the program Implemented successfully?
e. Has the program Maintained its performance?
iii-
Focus the evaluation design(Prevention &
Population Health Branch, 2010)
I will recommend an observational study design before and after the intervention to see its effect on the incidence of cervical cancer.
I will use the existing data collection tools i.e. the District Health Information System, Pakistan.
I will perform both the process and the outcome evaluation.
In the process evaluation I will record the number of activities done, attendance of the stakeholders, minutes of meetings and the reach of the program (Prevention and population council, 2010)
In the outcomes evaluation I will recommend a randomized control trial along with a qualitative study.
iv-
Data collection
Assign the task of data collection to individuals, remind them and provide them with incentives (Round et al, 2005)
v-
Data analysis and interpretation
In data analysis we get the results of the data collected/generated and come to know what the important findings are (Round et al, 2005)
vi-
Disseminate lessons learned
The lessons that are learned as a result of
evaluation must be disseminated for better use via trainings, presentations, publications,
administration and information technology for change towards better (Prevention
and population Health Branch, 2010)
Reference:-
Basu P, et al.(2009). Asian Cervical
Cancer Prevention Advisory Board. Journal of Obstetrics and Gynaecology .Res 2009;35:712–716.
Craig et al & Moore GF et al (2008). Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350:h 1258.
Economic Survey of Pakistan (2009-10) Chapter 10. Education. Available at: http://finance.gov.pk/survey/chapter_10/10_Education.pd Accessed on 21/06/2016
Green J., Tones K. et al (2015). Health promotion- planning and strategies. Third edition. London: Sage
Green LW & Kreuter MW (1999). Health promotion planning: an educational and ecological approach. 3rd Edn. California, Mayfield. Available at http://Igreen.net/precede.htm Accessed on 21/06/2016
Human Papilloma Virus and related Diseases Report, Pakistan
(2016). Version posted on www.hpvcentre.net
in Feb. 26, 2016; Available at: http://www.hpvcentre.net/statistics/reports/PAK.pdf
Accessed on 02/06/2016
Pakistan Demographic Health Survey
2012-2013.
Pal Sadia Ahsan (2015). Cervical
cancer prevention in Pakistan, Editorial. JSOGP 2015, Vol.5, No.2; Available at: http://jsogp.net/Volumes/Volume5-2/Cervical%20cancer%20Prevention%20in
Accessed on 28/05/2016
Prevention and Population Health Branch (2010). Evaluation framework for health promotion and disease prevention programs. Melbourne, Victoria Government Department of Health. Available at: www.health.vic.gov.au/healthpromotion/evidence_evaluation/cdp_tools.htm Accessed on 19/06/2016
Raza et al. (2010). HPV infection in
women with or without cervical cancer in Karachi, Pakistan. British Journal of
Cancer 2010; 102: 1657-1660.
Romanowski B, Schwarz TF, Ferguson LM,
Ferguson M, Peters K, Dionne M et al (2014). Immune response to the HPV-16/18 AS04-adjuvanted vaccine
administered as a 2-dose or 3-dose schedule up to 4 years after vaccination.
Hum Vaccin Immunother 2014;10 (5):1155-1165. doi: 10.4161/hv.28022
Round R, Marshall B & Horton K. (2005) Planning for effective health promotion evaluation. Melbourne, Victorian Government Department of Human Services. Available at: http://www.health.vic.gov.au/healtpromotion/evidence_res/integrated.htm Accessed on 19/06/2016
WHO Position Paper (April 2009);
Available at: www.who.int/immunization/documents/positionpap
ers/en/index.html Accessed
on 28/05/2016



Comments
Post a Comment